

The American Optometric Association (AOA) guidelines recommend referral for symptomatic retinal breaks for prophylactic laser treatment in many cases. Variable accompanying signs, symptoms, risk factors and break types need to be considered to make the proper recommendation (see tables 1-3). It has been documented that the overall clinical picture, including the type of break and symptomatology, are critical prognostic indicators for the development of RRD. Since then, several studies have evaluated the natural progression of retinal breaks. Therapy of retinal breaks started in 1920, when Gonin’s work led to the recognition that a retinal break was the cause of an RRD and that treatment of the RRD would require the sealing of such breaks.9 In 1950, with the advent of the xenon laser, prophylactic treatment of all retinal breaks was recommended to prevent an RRD.

About 30% of symptomatic, untreated retinal breaks result in an RRD. Referring our patient for immediate treatment was a critical step in safeguarding her vision. The lattice inferior area in the left eye and few retinal holes throughout left eye were also treated by the laser. We made a STAT referral to a retinal specialist, who lasered both the large retinal tear in the superior periphery of the right eye and the small retinal tear adjacent to the lattice superiorly of the left eye (figures 2 and 3). A retinal tear was noted adjacent to the area of the superior lattice. The periphery of the left eye showed areas of lattice degeneration in both the superior and inferior aspects, including scattered pigmented retinal holes throughout. The left eye revealed moderate syneresis and a second PVD. Scattered atrophic retinal holes were also observed throughout the periphery. A large retinal tear was evident in the superior retina of the right eye (figure 1). and O.S.ĭilated fundus examination of the right eye revealed a posterior vitreal detachment, associated with Schaeffer’s sign and an inferior vitreal hemorrhage. Intraocular pressure (IOP) was measured via Goldmann applanation tonometry at 16mm Hg O.D. Examination of the anterior segment was unremarkable. Her blood pressure measured 130/80mm Hg at 9:13 a.m. We determined that her best-corrected visual acuity was 20/20, O.D. She was not taking any systemic medications. Her systemic history was positive for hypercholesterolemia, which was controlled with diet and exercise. Superior retina of the patient’s right eye. 3-5 Any retinal break can allow passage of liquefied vitreous to gain access into the subretinal space, culminating in an RRD.

2 Up to 15% of patients presenting with acute PVDs have concomitant retinal breaks. The incidence of retinal breaks is highest during the sixth and seventh decade of life, when PVDs are more prevalent. 1 During a PVD, traction at a site of firm vitreoretinal adhesion may lead to the development of a retinal break. The pathogenesis of an RRD may be variable but an acute posterior vitreous detachment (PVD) is commonly the cause.Ī total of 67% of patients older than 65 years of age develop a PVD, but most experience no adverse sequelae. The detachment requires a full-thickness retinal break, vitreous traction and the passage of fluid through the break. The two classifications of retinal detachment, which differ based on underlying etiologies, include tractional/exudative (also known as serous) and hegmatogenous retinal detachment (RRD). Here, we discuss many aspects of these complex cases.Ī retinal detachment is a separation of the neurosensory retina from the retinal pigment epithelium (RPE). Although some patients require an urgent response, others may need prophylactic therapy, monitoring or some other approach.
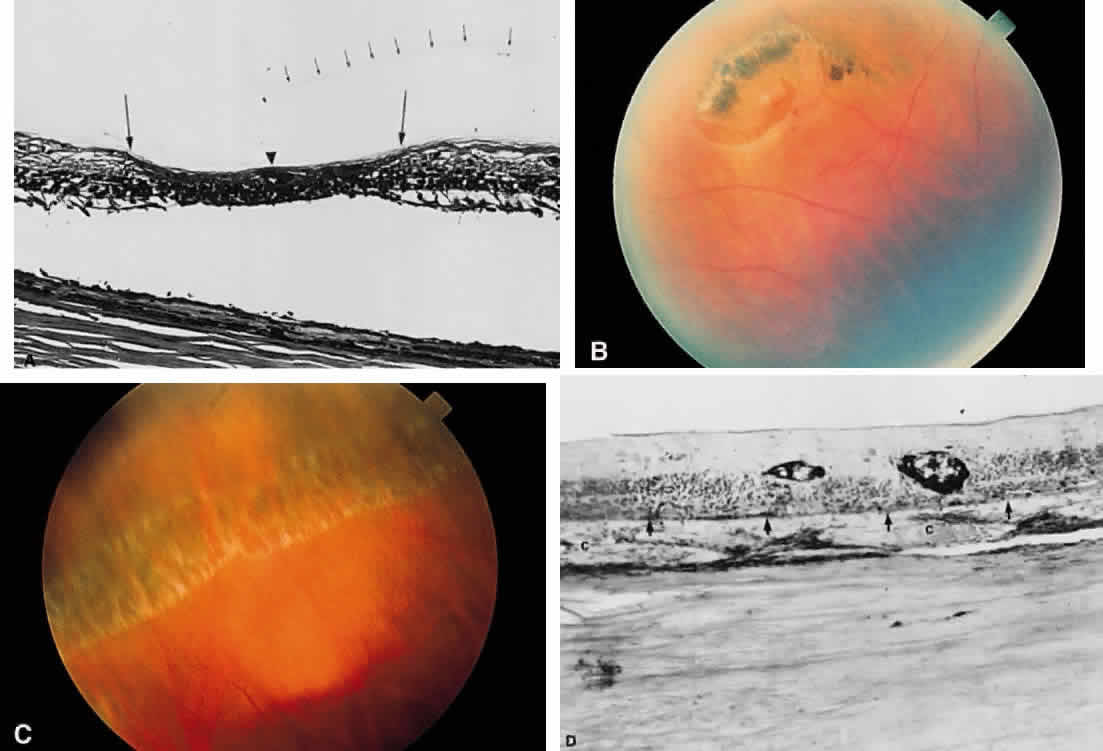
Our patient’s case showcases one of many different types of retinal tears that you may encounter in practice. Fortunately, laser treatment was arranged-but only after initial work-ups and treatment failed to address her most serious problem. Testing eventually confirmed a horseshoe retinal tear that required emergency intervention. The patient reported seeing flashes that had subsided in the same eye three months earlier. A 61-year-old Hispanic female, presented to our primary care clinic with a chief complaint of right eye floaters that had degraded her vision during the previous four days.


 0 kommentar(er)
0 kommentar(er)
